Pelvic girdle pain (PGP) also commonly known as pelvic instability effects up to 50% of women during pregnancy.
Thankfully, 90% of women recover from PGP within 12 months of having their baby.
However, up to 10% of women can continue to have significant PGP and disability 2 years post-birth.

PGP often refers to pain that is experienced either at the back of the pelvis at the sacroiliac joint and/or pain over the pubic symphysis at the front of the pelvis.
Pain may be referred into the buttock and/or down the leg (sometimes mistaken for sciatic pain), groin, and inner thigh, lower abdominal and vaginal area.
What causes PGP?
There is generally little movement in the pelvis when you are not pregnant; this is helped with the support of ligaments and muscles.
The role of the pelvis is to transfer weight from the leg to the trunk back to the other leg when we are walking; increased load such as carrying weight/pregnancy or jogging/running significantly increase the load on the joint as well as its ability to transfer the weight effectively.
During pregnancy hormonal changes occur that effect the laxity of the ligaments which result in a slight increase in movement in the pelvis.
This laxity is required to increase the width of the pelvis in order to deliver a baby through it.
This increased movement although small can be double of what was there previously increasing the stress on the ligaments and resulting in inflammation and pain.
The muscles that support the pelvis, if working correctly will recognise the increased movement in the joint and help maintain good control of the pelvis.
However, commonly in pregnancy these muscles do not recognise the need to change the way they work resulting in poor control of the extra movement leading to increased stress on the joint, inflammation and pain.
Other changes that occur during pregnancy that can increase the stress on the pelvis include:
- Stretch of the abdominal muscles as the baby grows
- Increased weight of the baby on the pelvic floor throughout the pregnancy resulting in a slight stretch of the muscles (similar to a trampoline with a child on it)
- Change in your centre of gravity resulting in increased load on your back.
Common symptoms
Symptoms can range from mild to severe but are treatable at any stage of pregnancy. Early treatment can prevent sever disability later in pregnancy.
Some symptoms experienced include:
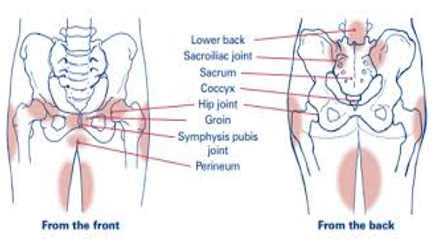
1. Pain in the pubic region, back of pelvis, lower back, hips, groin or thighs
2. Pain made worse by movement, for example:
- walking on uneven surfaces,
- getting in and out of the car
- standing on one leg
- climbing the stairs
- getting in or out of bed or rolling over in bed
- Pain during sexual intercourse.
- Running
- Pushing a shopping trolley (worse when it is fully loaded).
- Vacuuming / mopping.
- Carrying a toddler on your hip;
Treating symptoms
As previously described symptoms of PGP relate to inflammation around the joint, therefore the initial treatment (first 48hrs) is the same as that for a sprained ankle.
- Ice – Helps settle inflammation. Apply for 20min every 2 hours. You don’t need to wake up in the middle of the night to apply the ice. However, if you wake up due to pain the application of ice can help settle your pain and allow you to fall back asleep.
- Rest – Rest for 1-3 days depending on the severity of your condition. This means you need to be sitting or lying for most of the day. Use pillows between your legs and under your tummy as needed. After this initial rest period it is important to begin exercise. Specific exercises prescribed by your physiotherapist will insure that the muscles required to support and control your pelvis are working optimally. Without exercise these muscles will continue to get weaker and your pelvic pain will continue to worsen as your pregnancy progresses.
Treating cause
Pain and inflammation have the ability to change how the body uses muscles in that area.
Sometimes this can cause a delay in these muscles switching on or not switching on all together.
As a result the larger muscle groups will all switch on to splint the joint resulting in muscle spasm or a new pain, i.e. lower back pain, inner thigh, gluts, hamstrings or hip flexors.
Your physiotherapist will provide a thorough assessment of your movement, stability and strength.
They will also treat muscle spasm and give you advice on how to manage this at home.
They will also prescribe specific exercises to insure that the muscles responsible for maintaining movement and stability in the pelvis are working optimally.
Physiotherapists may also prescribe extra support in the form of belts, tube grip or pregnancy shorts.
It is important that you only use these devices if prescribed as they will not be appropriate for every women and they need to be fitted correctly to avoid any further aggravation of symptoms.
Other treatment options include:
- Hydrotherapy (pool based exercise)
- Warm bath, heat pack or cold pack
- Acupuncture
Exercise
1. Cardio
- Pain free walking on even surface in comfortable and supportive foot wear.
- Swimming: Is great for PGP as it is non weight bearing however breaststroke should be avoided to reduce any increased pressure on the pelvis.
- Cycling: on a stationary bike to reduce risk of falls and trauma. Also insure the bike is set up correctly i.e handle bars are high to accommodate for tummy, and knees are at approximately 30 degree bend. Insure you have good pelvic control and that you apply even pressure through both peddles.
2. Pilates
- Great for overall strength and focuses on the core muscles that help support the pelvis and lower back.
How will it affect your delivery?
Most women with PGP will be able to go on and have a vaginal delivery.
Your physiotherapist will be able to guide you through the best labour positions and strategies for birth.
Post-birth
The good news is that 90% of women will make a full recovery within 3-12months post giving birth.
During this time it important to continue with exercise prescribed by your physiotherapist and be aware of your posture.
If you are breastfeeding, hormones that cause laxity in your ligaments remain high therefore your pelvis will still be subject to increased movement.
The future
Many women are told that once you have had PGP in one pregnancy, you will get it again next pregnancy, but earlier and possibly worse.
This is very possible and highly likely.
However, research shows that if you rehabilitate and recover well after your baby is born, the results gained in the first 6 months are maintained for one to two years later.
Remember your body has just run a 9 month long marathon, time to recover and rehabilitate is essential.
This will help in reducing your risk of PGP in subsequent pregnancy’s and /or developing pelvic floor dysfunction such as urinary incontinence (bladder leakage) but more about that later.
If you have any further questions please feel free to call (08) 9384 3269 or book an appointment online.
