Osteoarthritis (OA)
What is OA?
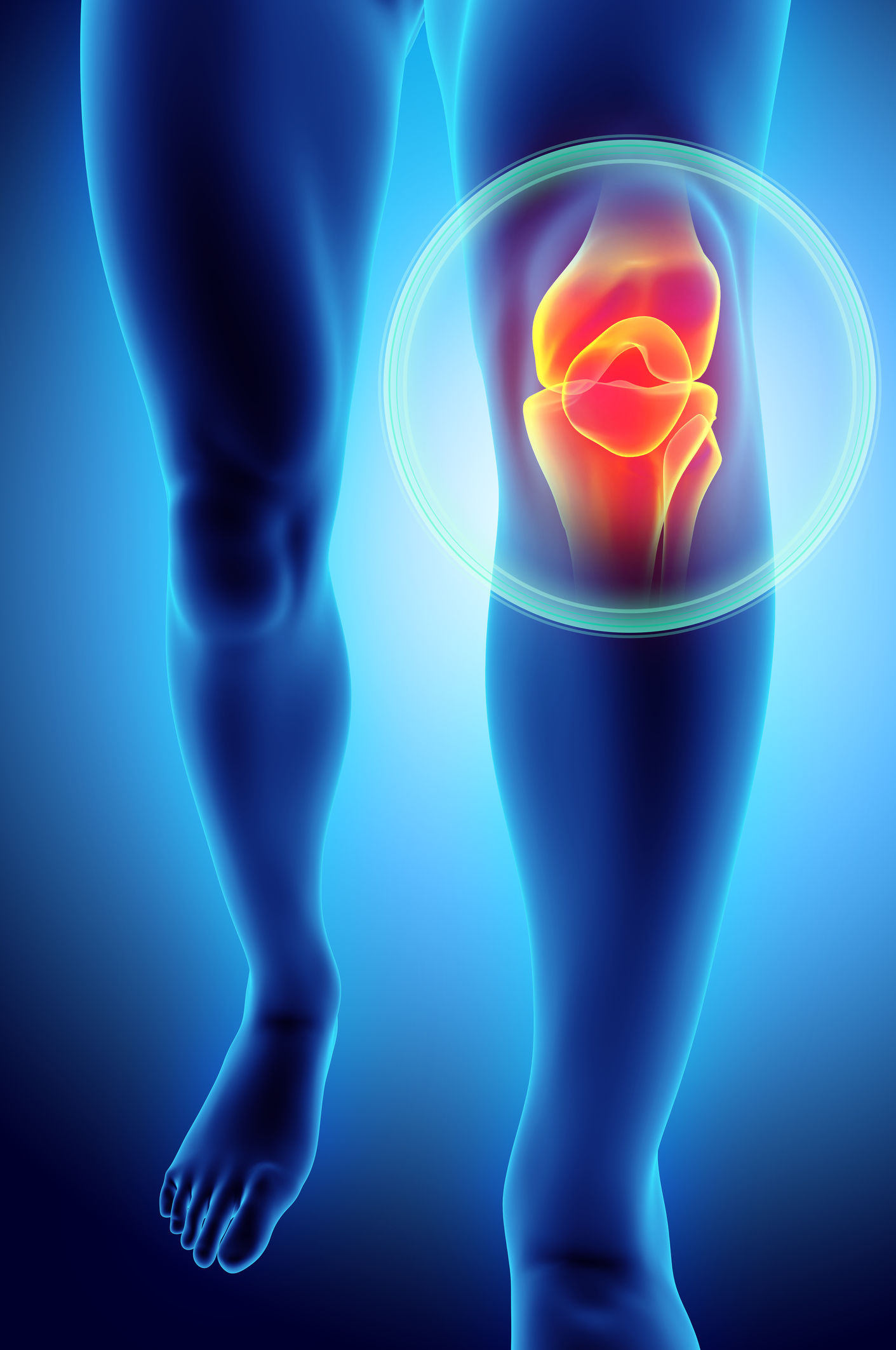
Osteoarthritis is often described as a ‘wear and tear’ process, when in fact OA is better understood as a condition which affects the whole joint, resulting in weaker muscles, irritated ligaments and altered biomechanics/movements as well as a reduction in the thickness of the cartilage. It can affect any joint with a cartilage, but most commonly occurs in the hips, knees, and hands.
In a healthy joint, the cartilage allow bones to glide smoothly over each other and also acts as a shock absorber. The cartilage is nourished and healed through movements and putting weight through the joint (e.g. walking, running, stairs) and can be damaged if there is too little or too much force being put through the joint. OA generally occurs when the amount of damage is greater than the amount of nourishment for a long period of time (years!).
What are the symptoms?
Commonly reported symptoms include:
- Pain
- Joint stiffness
- Swollen joints
- Feelings of instability or ‘giving way’
- Clicking or cracking sound with movement
What are the risk factors?
- Age
- Gender (Females > Males)
- Obesity
- Previous trauma to the joint
- Physical inactivity
- Joint overloading
How is OA diagnosed?
OA is commonly diagnosed by a health professional considering reported symptoms (aching, clicking, stiffness, giving way) and a thorough clinical examination. An X-ray may show the narrowing and structural changes in the joint, however findings on an x-ray are not often not proportional to the person’s symptoms (ie. Less cartilage does not necessarily mean more pain). As such an X-ray alone is not enough to diagnose OA.
How do you treat OA?
Education
Having a comprehensive understanding of joint movement and what factors will either help or hinder a joint with OA will assist in making some lifestyle modifications to help manage your pain and make day to day tasks easier. As the cartilage needs to be appropriately loaded for it to be healthy, exercise has been consistently found to help improve joint range and stability to improve overall function. Exercise does not do further damage to the muscles and joints!
Exercise
Exercise is a type of physical activity carried out with a specific purpose, such as getting stronger, moving better or improving flexibility. It is different from physical activity which refers to any body movement that makes the heart beat faster (e.g. lifting heavy boxes at work). To specifically improve a joint with OA, exercise should be performed whilst concentrating on the position and alignment of your joints in order to load the joint optimally. You should exercise at a level that suits your fitness level to see improvements and prevent injuries!
Weight loss
Obesity is one of the key factors which increase your risk of developing OA. For every extra kilo your body carries, the amount of force going through your leg with each step increases by 3-5 kgs! Weight loss helps to reduce the stress and pain on the joint and makes further exercise easier.
Other Options
Other treatments like pain relieving medications, aids (braces/supports/crutches), and passive treatments by a therapist (massage, joint mobilisation) should not be used in isolation. These modalities should only be used to help assist with daily exercises!
Surgery – The Last Resort
Surgery, like total joint replacements, should only be used as the last resort for severe OA when exercise and other treatments have not been sufficient. 80-90% of people experience some pain relief after undergoing surgery and the completing a subsequent rehabilitation process, but that leaves another 10-20% of people who do not see any benefits of surgery. As per any surgery, there are also side effects associated with it.
Is there a cure for OA?
There is currently no cure for OA. However studies have shown that exercise therapy produces the best result in managing pain and improving function.
What can physiotherapy do for OA?
Physiotherapists are experts in designing and progressing personalised exercise programs to specifically address the pain, stiffness and other symptoms caused by OA, taking into account an individual’s goals and current level of function. Julia Lee and Jordan Wilson have undergone further training in the treatment and management of OA through the internationally recognised GLA:D program and are happy to answer any questions you have about OA!