Jonathan Tan, Senior Physiotherapist at Lifecare Point Walter.
Low back pain is a very common problem that most people will experience at least once in their lifetime.
However, one of the biggest misconceptions in society surrounding low back pain is that we should avoid bending, particularly when experiencing a flare up.
In some cases this may be true, for example:
- In acute low back pain when forward bending significantly flares pain
- In cases of radicular pain when bending significantly aggravates leg pain or neurological symptoms such as pins and needles
However, although in both cases avoiding forward bending may be beneficial in the early stages, it’s important to progressively regain normal lumbar flexion.
Continuing to avoid flexion is likely to become a barrier to a full recovery.
So let’s say you’ve just strained your back.
You went to pick a piece of rubbish off the floor and suddenly felt a strain across your lower back.
Over the next hour the pain progressively increased and your back began to feel tighter and tighter.
The pain is moderate to severe with forward bending, prolonged sitting and particularly when getting up from sitting to standing.
What now?
When is it safe to start bending?
Early in my physiotherapy career, I would likely have advised to continue moving and walking regularly through the day, avoid prolonged sitting, use a heat pack and avoid forward bending for 1-2 days.
To look at things very simply, I think in this acute situation things can go one of two ways.
Gentle repeated flexion (bending) may aggravate the pain or it may actually relieve it when performed in supported and less threatening positions.
Here are a couple of exercises to try day 1-2:
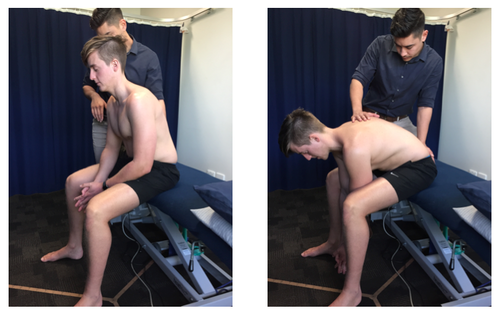
Seated lumbar flexion
Child’s pose


So how do I know whether to continue bending or to avoid it?
When performing the exercise (let’s say seated lumbar flexion) what happens?
It’s normal to expect the movement to be painful initially, however if the pain is mild to moderate I would say it’s safe to continue.
Gently and progressively work further into flexion, without sustaining the position for any longer than a couple of seconds.
If the pain continues to get worse – STOP!
- This may suggest it’s still too early to begin bending to this degree
- It may be a good idea to apply some strapping tape to the lumbar spine for a couple of days to avoid any excessive flexion. We can come back to this exercise/test later.
If the pain starts to ease and you notice you can progressively move further – keep going!
- If things are feeling better, why stop?
- We still want to set a limit, in case you have a delayed pain response
- To keep it simple aim for 3 x 10-15 repetitions a few times in the day
What is the best position to sit?
In acute low back pain, prolonged sitting is quite often an aggravating activity.
However, again I think too much emphasis has been put on avoiding flexion and bending the spine when sitting.
Sitting upright forces the lumbar erector spinae muscles to activate and a lot of endurance is required to maintain this position for long periods of time.
If these muscles are already in spasm, sitting too upright may further aggravate pain.
We need to relax these muscles.

If you’re experiencing low back pain, sit in the position that is most comfortable for you.
If relaxing your low back muscles and slightly slumping is relieving, than go for it.
Maybe sit with a pillow to prevent you from slumping too far, but enough to still let you actually relax!
It’s more likely the long periods of time in sitting that aggravate the problem, so try to get up and walk around regularly.
What’s actually happening?
In acute low back pain, the only musculoskeletal structure that has the capacity to cause such a dramatic decrease in lumbar flexion range in a short amount of time is muscle.
Our muscles will go into spasm as a protective mechanism to avoid us from moving too far into a painful position.
However, muscle spasm will often happen in the absence of any significant structural pathology, e.g. large disc protrusion, therefore chasing an improvement in lumbar flexion early may well be quite safe.
Muscle spasm itself can cause a lot of pain both from the muscle as a source of pain as well as the compressive load this muscle spasm applies to the spine.
Progressively relaxing this muscle spasm through normal movements can be very effective.
Progression – why am I still stiff?
It is important to continue to bend and improve our lumbar flexion range.
Following a lumbar strain, many people continue to say they are experiencing stiffness in their back.
Why is this though?
It’s reasonable to expect our muscles should have relaxed and returned back to their normal length by then. Our vertebrae certainly can’t degenerate to that extent in such a short period of time.
Here’s a link to an interesting article I read which may help to explain why many people continue to feel stiff.
Stanton et al (2017) performed a study that found a ‘feeling of back stiffness’ correlated poorly to biomechanical measures of back stiffness.
Rather, many people develop a protective response to avoid movement to prevent provocation or injury.
‘Feeling stiff’ is an important predictor of disability but if this is primarily driven by a fear of movement, this must be addressed.
In most cases, pain does not indicate you’re doing damage. It’s important to regain your movement!
Final thought
The main point I want to make here, is that it’s safe to bend.
In the acute stage of low back pain, I think our brains perceive forward bending in standing as serious no-go.
Likely because the strain occurred initially with this movement or because we’re less stable than in sitting or on all fours.
Bending in a more supported position like sitting may help to modify that neuromuscular response to spasm and actually recover faster.
Keep in mind, this may not apply to everyone with low back pain.
When there is clearly a strong inflammatory process or dominant neuropathic pain, avoiding bending may be best.
In any case it’s best to speak to your physiotherapist when this type of pain occurs.
If you are experiencing lower back pain, you can book an appointment with your local Lifecare physiotherapist.

